Download our free and printable SOAP note templates word which are available below at the end of this page. The SOAP note, which is an abbreviation of Subjective, Objective, Assessment and Plan is a method of certification adopted by health care providers to prepare notes in a patient’s chart, with other common formats, like admission note. We do hope that you will like these SOAP note templates at this page.
It provides information about the patient which is written and presented in a particular way, and includes specific factors. SOAP notes are widely used for admission notes, medical records, and several other documents in a patient’s table. Throughout the world, various healthcare clinicians including nurses, physical and occupational therapists, athletic trainers, counselors and doctors use these type of notes.
Furthermore, if you are a medical student you will probably require to use a SOAP note format. The major purpose of creating this note is to have a standard layout for organizing patient’s information.
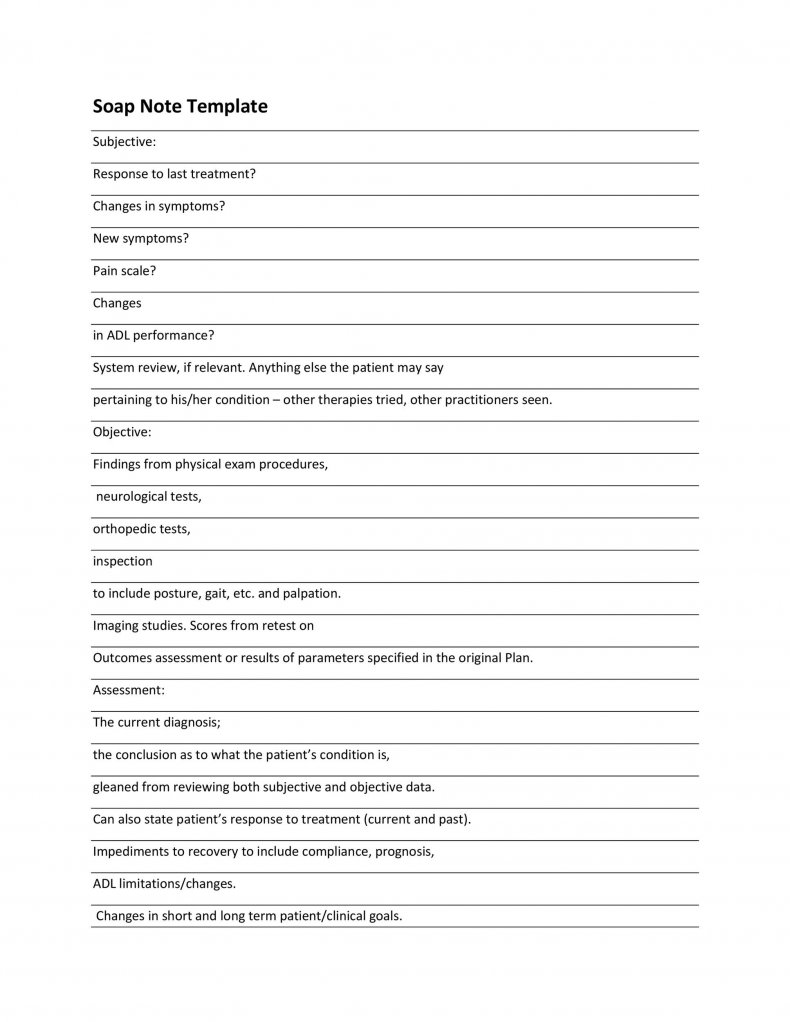
Each section of SOAP note requires particular information, including subjective, which refers to subjective observations that are orally expressed by the patient, objective part consists of objective observations, assessment is the diagnosis or condition the patient’s suffering from, the last section called plan, which refers to the way you are going to address the patient’s problem.
It may also include treatment that is recommended like medication or surgery. Nevertheless, in order to assure that patient gets the perfect treatment, various hospitals prefer to employ the SOAP analysis by creating such note.
By following our SOAP note templates word will help you create a standard and organized way of documenting all patients’ information enabling the professional to collect information about a patient, and make a conclusion about what is wrong and how to treat it. Download these SOAP note templates word given below.